Preventing Pelvic Organ Prolapse: Tips and Tricks for a Stronger Pelvic Floor
Pelvic organ prolapse is a common condition that affects many women. It occurs when the muscles and tissues that support the pelvic organs become weak or damaged, causing the organs to drop down and press against the vaginal wall. This can lead to uncomfortable symptoms such as pelvic pressure, discomfort, and incontinence.
Understanding Pelvic Organ Prolapse: Causes, Symptoms, and Risk Factors
Pelvic organ prolapse occurs when the muscles and tissues that support the pelvic organs become weak or damaged. This can happen for a variety of reasons, including childbirth, menopause, and aging. During childbirth, the pelvic floor muscles can become stretched or torn, which can weaken their ability to support the organs. Menopause can also contribute to prolapse, as the decrease in estrogen levels can cause the tissues to become less elastic. Aging can also play a role, as the muscles and tissues naturally weaken over time.
Symptoms of pelvic organ prolapse can vary depending on the severity of the condition. Some women may experience no symptoms at all, while others may experience discomfort, pressure, or a feeling of fullness in the pelvic area. In more severe cases, the organs may protrude from the vaginal opening. Risk factors for pelvic organ prolapse include obesity, chronic constipation, and a family history of the condition.
Pelvic Organ Prolapse (POP) is "vaginal bulge" due to weakness of the pelvic floor, or muscles in the vagina.
SYMPTOMS:
The symptoms of pelvic organ prolapse can vary depending on the specific organs involved. Common symptoms may include:
- A feeling of pressure or fullness in the pelvic area
- Sensation of something bulging or protruding from the vagina
- Urinary problems, such as frequent urination, urine leakage, or difficulty emptying the bladder
- Bowel issues, including constipation or difficulty with bowel movements
- Sexual discomfort or decreased sexual sensation
- Lower backache or pelvic pain
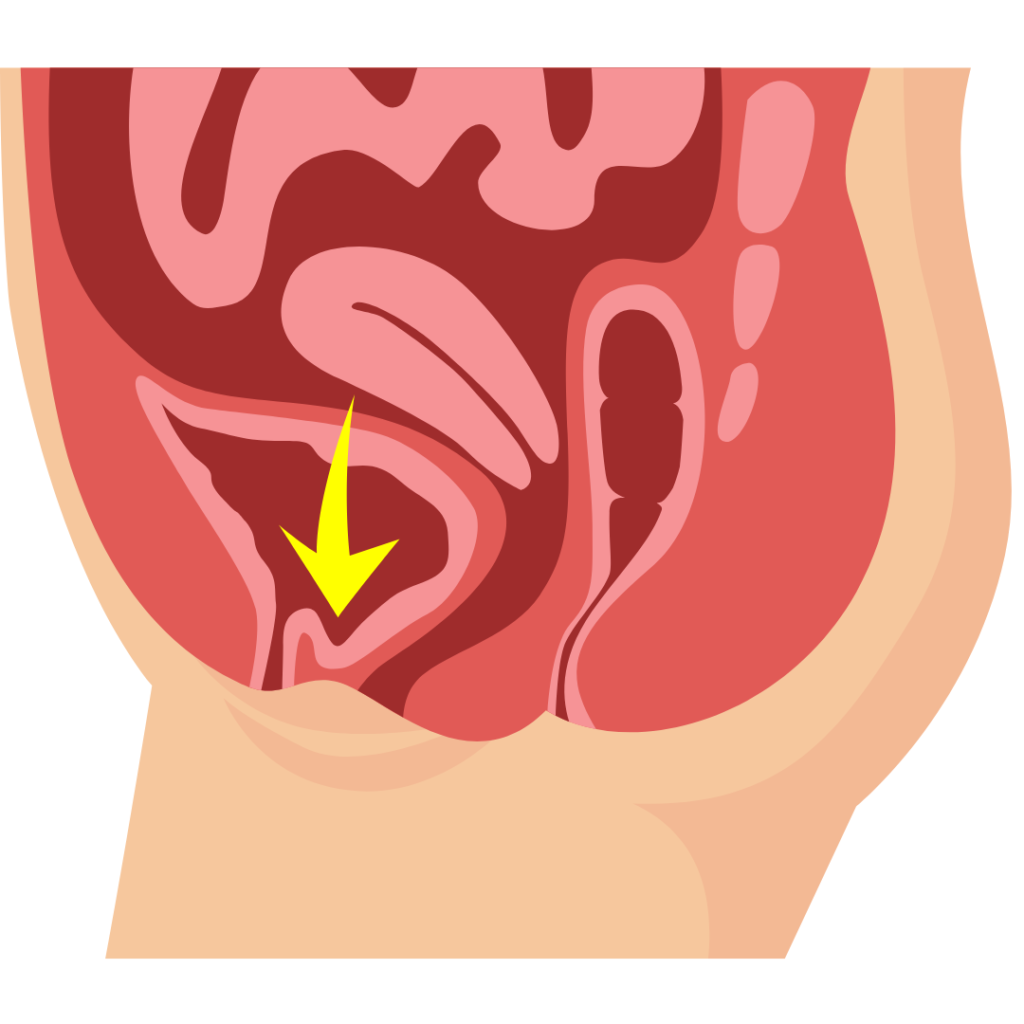
ANTERIOR PROLAPSE OR CYSTOCELE
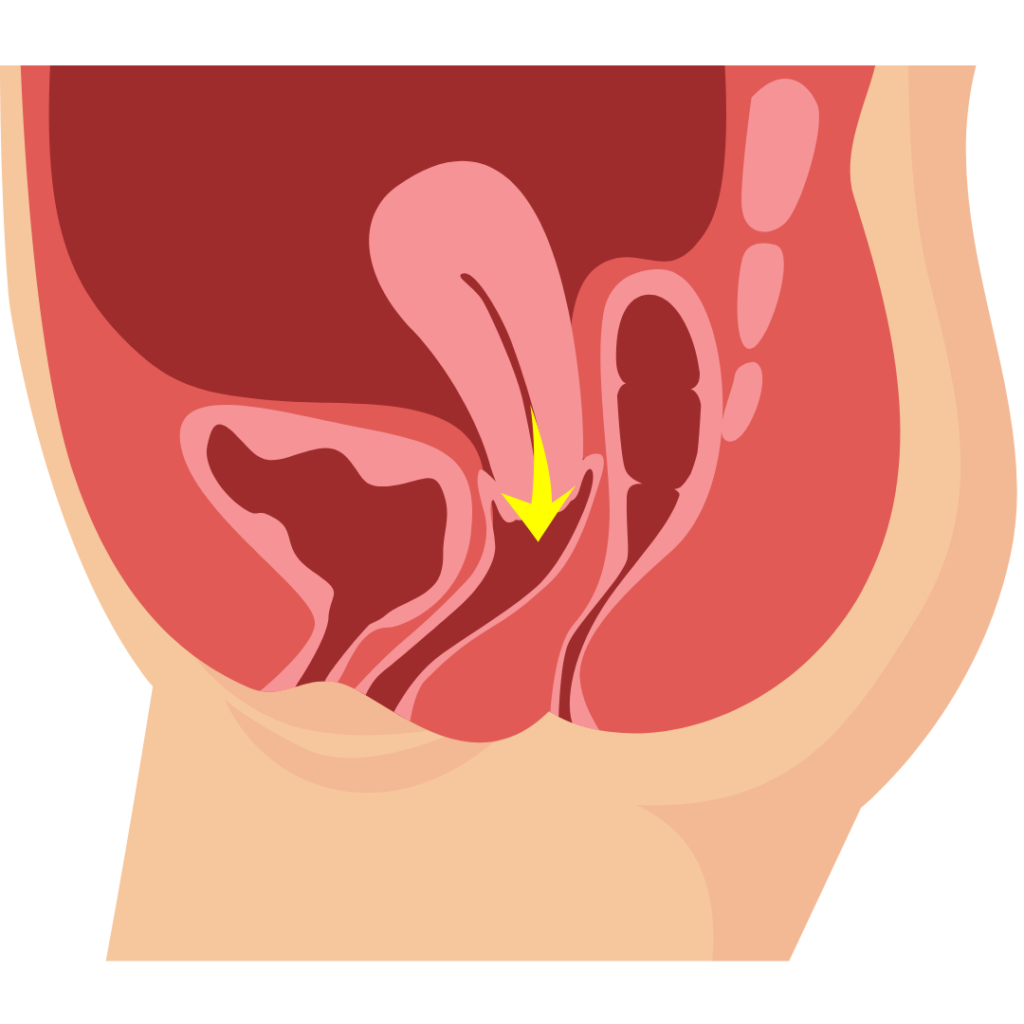
APICAL PROLAPSE OR ENTEROCELE
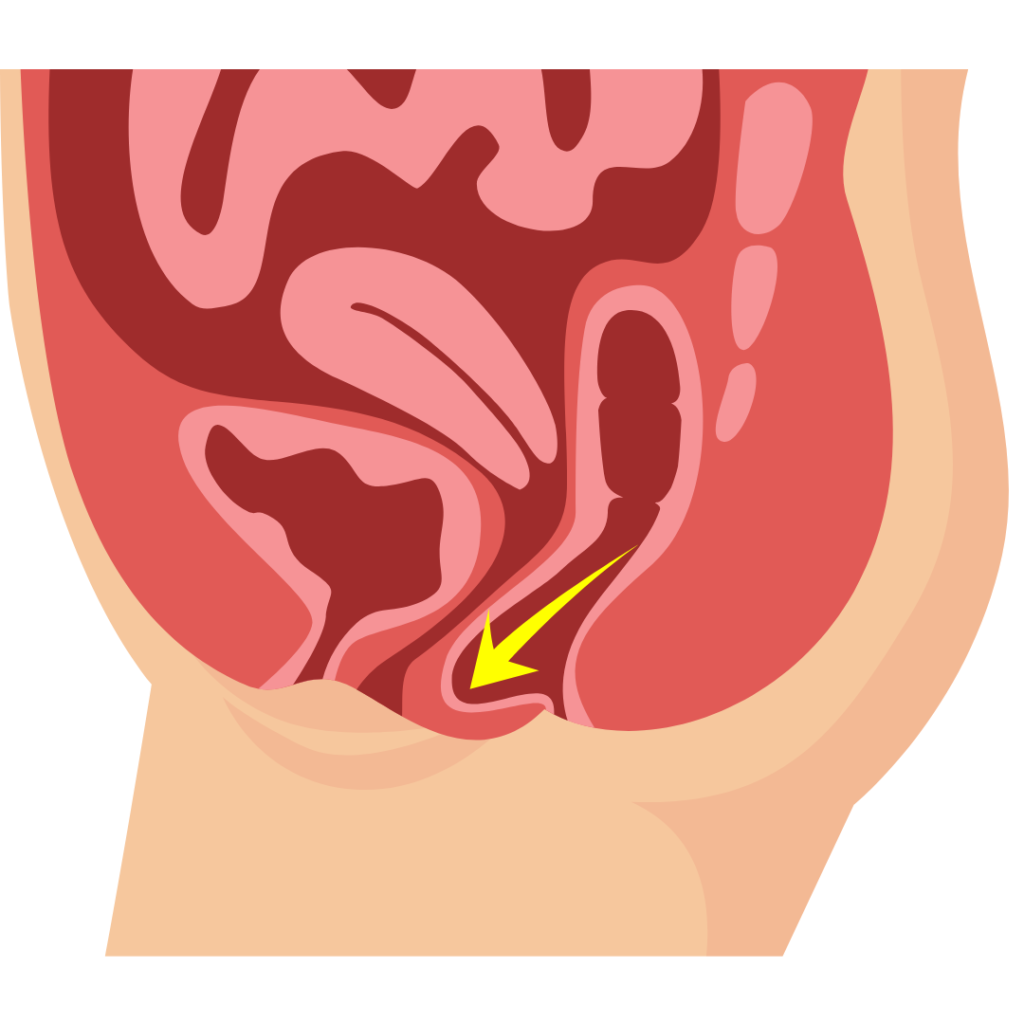
POSTERIOR PROLAPSE OR RECTOCELE
Causes
Pelvic organ prolapse can be caused by various factors, including:
- Pregnancy and childbirth: The strain placed on the pelvic floor muscles during pregnancy and vaginal delivery can weaken them over time.
- Aging: The natural aging process can lead to the gradual weakening of pelvic support structures.
- Menopause: Reduced levels of estrogen after menopause can contribute to pelvic floor muscle weakness.
- Chronic coughing or heavy lifting: These activities can put pressure on the pelvic organs and weaken supporting tissues.
- Genetic factors: Some women may have a genetic predisposition to developing pelvic organ prolapse.
- Connective tissue disorders: Certain conditions affecting connective tissues, such as Ehlers-Danlos syndrome, can increase the risk of prolapse.

How do you diagnose POP?
If you suspect pelvic organ prolapse, it is important to consult with a healthcare professional, typically a gynecologist or urogynecologist, for a proper diagnosis. The following diagnostic methods may be used:
Medical history: Your doctor will ask questions about your symptoms, medical history, pregnancies, and lifestyle factors.
Physical examination: A pelvic exam will be performed to assess the extent of the prolapse and identify the specific organs involved.
Additional tests: In some cases, additional tests may be recommended, such as urodynamic studies to evaluate bladder function or imaging tests like MRI to assess pelvic structures.
The Importance of a Strong Pelvic Floor: How It Can Prevent Prolapse
The pelvic floor muscles play an important role in supporting the pelvic organs and preventing prolapse. When these muscles are weak, they are less able to support the organs, which can lead to prolapse. Strengthening the pelvic floor muscles can help prevent prolapse and improve bladder control and sexual function.
Kegel Exercises: A Pelvic Floor Strengthening Technique
Kegel exercises are a simple and effective way to strengthen the pelvic floor muscles. To perform Kegels, simply contract the muscles that you would use to stop the flow of urine, hold for a few seconds, and then release. Repeat this exercise several times a day, gradually increasing the length of time that you hold the contraction. Start by doing them lying down twice a day and then gradually change your position to sitting and then standing as your muscles become stronger. It is important to perform Kegels correctly in order to get the most benefit from them.
Diet and Lifestyle Changes to Support Pelvic Floor Health
Maintaining a healthy diet and lifestyle can also help support pelvic floor health. Eating a diet rich in fiber can help prevent constipation, which can contribute to prolapse. Avoiding smoking and managing chronic conditions such as diabetes can also help improve pelvic floor health.
The Role of Weight Management in Preventing Pelvic Organ Prolapse
Maintaining a healthy weight is also important for preventing pelvic organ prolapse. Excess weight can put extra pressure on the pelvic floor muscles, which can weaken them over time. Losing weight can help reduce this pressure and improve pelvic floor health.
Avoiding High-Impact Exercises and Activities That Can Strain the Pelvic Floor
High-impact exercises such as running and jumping can put extra strain on the pelvic floor muscles, which can contribute to prolapse. It is important to avoid or modify these exercises if you are at risk for prolapse. Low-impact exercises such as swimming and cycling are safer options for the pelvic floor.
Proper Lifting Techniques to Avoid Putting Pressure on the Pelvic Floor
Improper lifting techniques can also put extra pressure on the pelvic floor muscles, which can contribute to prolapse. It is important to lift heavy objects safely, using your legs instead of your back, and to ask for help if you need it.
How to Use Pelvic Floor Physical Therapy to Treat and Prevent Prolapse
Pelvic floor physical therapy is a non-invasive treatment option for pelvic organ prolapse. During a pelvic floor physical therapy session, a trained therapist will work with you to strengthen the pelvic floor muscles and improve bladder control. This can help prevent prolapse and improve symptoms in those who already have the condition.
When to See a Doctor: Signs that You May Need Medical Intervention for Pelvic Organ Prolapse
If you are experiencing bothersome symptoms of pelvic organ prolapse, it is important to see a doctor. Severe discomfort or difficulty with daily activities may require medical intervention. Your doctor can help determine the best course of treatment for your individual needs.
TREATMENT
The treatment options for pelvic organ prolapse depend on the severity of symptoms, the impact on quality of life, and individual preferences. The following are common treatment approaches:
-
Conservative management:
Pelvic floor exercises (Kegel exercises) to strengthen the muscles supporting the pelvic organs.
Lifestyle modifications, such as weight management, avoiding heavy lifting, and treating chronic cough.
- Pessaries: These removable devices are inserted into the vagina to provide support for the pelvic organs.
- Surgical repair: This involves restoring the support structures and repositioning the pelvic organs to their normal position. Various surgical techniques may be used depending on the specific situation.
- Minimally invasive procedures: These include robotic-assisted surgeries, which offer smaller incisions and quicker recovery compared to traditional open surgeries.
- Hysterectomy: In some cases, if the uterus is contributing to the prolapse, removal of the uterus (hysterectomy) may be recommended.
- Watchful waiting: If the prolapse is not causing significant symptoms or affecting the quality of life, doing nothing or watching and waiting is completely safe and reasonable.
Pelvic organ prolapse is a common condition that can significantly impact a woman's quality of life. Recognizing the symptoms, understanding the causes, and seeking timely diagnosis and treatment are essential. With the right treatment approach, tailored to individual needs, many women can find relief from the symptoms and regain normal function. If you suspect pelvic organ prolapse, schedule an appointment (include link) to discuss your options and develop an appropriate treatment plan.
Recommended Videos
Topic 37: Pelvic Floor Disorders
Your Vagina is falling out…?! | Pelvic Organ Prolapse Symptoms
Pelvic Organ Prolapse
Pelvic Floor Training
Can you really do Kegel Exercises anytime, ANYWHERE…?!? | Pelvic Floor Physical Therapy